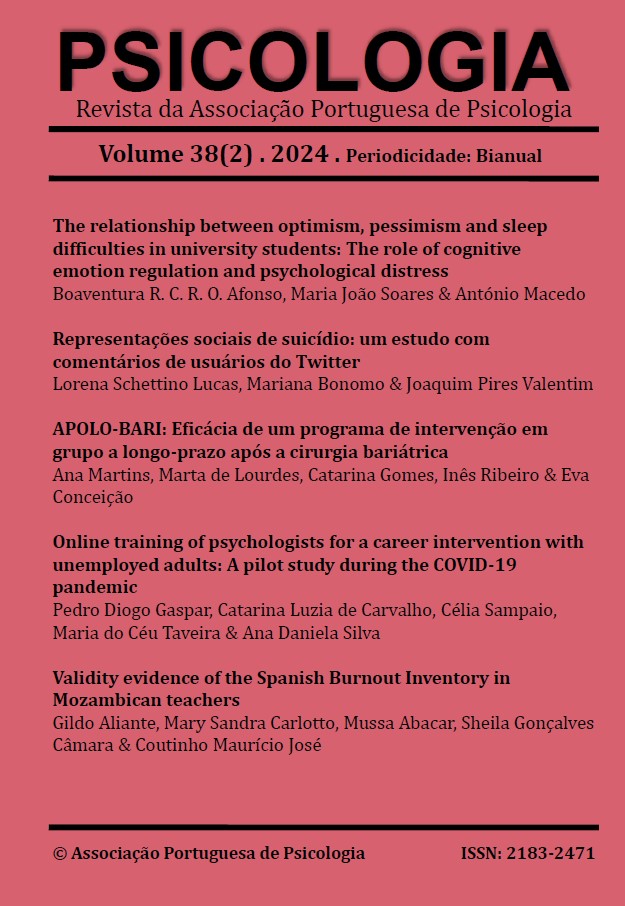
APOLO-BARI: Eficácia de um programa de intervenção em grupo a longo-prazo após a cirurgia bariátrica
DOI:
https://doi.org/10.17575/psicologia.1956Palavras-chave:
Ansiedade, Cirurgia Bariátrica, Depressão, Estudos de Acompanhamento, Perda de PesoResumo
Após a cirurgia bariátrica, alguns sujeitos podem experimentar a recuperação do peso a longo-prazo, devido a padrões alimentares problemáticos e ao reduzido número de consultas médicas na pós-cirurgia. Portanto, aponta-se a necessidade de um acompanhamento continuado nesse período. Surge então o APOLO-Bari, uma intervenção desenvolvida com o intuito de acompanhar e monitorizar os resultados pós-cirúrgicos. Tornou-se objetivo testar a sua eficácia, testar de que forma o TFEQ-21 se relaciona entre si e com as restantes variáveis e verificar se a adesão é um fator diferenciador dos resultados obtidos. O estudo inclui dois grupos: o de controlo (n = 113), que recebeu o tratamento usual pós-cirúrgico e o de intervenção (n = 38) que recebeu o tratamento usual e o APOLO-Bari. Verificaram-se reduções dos níveis de ansiedade, depressão, stress e de petisco contínuo no grupo de intervenção, contrariamente ao grupo de controlo. A adesão não impactou os resultados obtidos no final do programa.
Downloads
Referências
Abilés, V., Abilés, J., Rodríguez-Ruiz, S., Luna, V., Martín, F., Gándara, N., & Fernández-Santaella, M. C. (2013). Efectividad De La Terapia Cognitivo-Conductual En La Pérdida De Peso Tras Dos Años De Cirugía Bariátrica En Pacientes Con Obesidad Mórbida. Nutricion Hospitalaria, 28(4), 1109–1114. https://doi.org/10.3305/nh.2013.28.4.6536
Andreu, A., Jimenez, A., Vidal, J., Ibarzabal, A., De Hollanda, A., Flores, L., Cañizares, S., Molero, J., & Moizé, V. (2020). Bariatric Support Groups Predicts Long-term Weight Loss. Obesity surgery, 30(6), 2118–2123. https://doi.org/10.1007/s11695-020-04434-2
Bekker, M. H. J., Van de Meerendonk, C., & Mollerus, J. (2004). Effects of Negative MoodInduction and Impulsivity on Self-Perceived Emotional Eating. International Journal ofEating Disorders, 36(4), 461–469. https://doi.org/10.1002/eat.20041
Bertoletti, J., Galvis Aparicio, M. J., Bordignon, S., & Trentini, C. M. (2019). Body image and bariatric surgery: a systematic review of literature. Bariatric surgical practice and patient care, 14(2), 81-92. https://doi.org/10.1089/bari.2018.0036
Boniecka, I., Wilenska, H., & Jeznach-Steinhagen, A. (2017). Stress as a factor contributing to obesity in patients qualified for bariatric surgery. Videosurgery and Other Miniinvasive Techniques, 12(1), 60–67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5397539/pdf/WIITM-12-29073.pdf
Buchwald, H., & Consensus Conference Panel (2005). Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surgery for obesity and related diseases: official journal of the American Society for Bariatric Surgery, 1(3), 371–381. https://doi.org/10.1016/j.soard.2005.04.002
Cassin, S. E., Sockalingam, S., Du, C., Wnuk, S., Hawa, R., & Parikh, S. V. (2016). A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behaviour Research and Therapy, 80, 17–22. https://doi.org/10.1016/j.brat.2016.03.001
Chan, J. K. Y., King, M., & Vartanian, L. R. (2020). Patient perspectives on psychological care after bariatric surgery: A qualitative study. Clinical Obesity, 10(6), 1–9. https://doi.org/10.1111/cob.12399
Colles, S. L., Dixon, J. B., & O'brien, P. E. (2008). Grazing and loss of control related to eating: two high‐risk factors following bariatric surgery. Obesity, 16(3), 615-622. https://doi.org/10.1038/oby.2007.101
Conceição, E. M., Machado, P. P. P., Vaz, A. R., Pinto-Bastos, A., Ramalho, S., Silva, C., & Arrojado, F. (2016). APOLO-Bari, an internet-based program for longitudinal support of bariatric surgery patients: Study protocol for a randomized controlled trial. Trials, 17(1). https://doi.org/10.1186/s13063-016-1246-z
Conceição, E. M., Mitchell, J. E., Engel, S. G., Machado, P. P. P., Lancaster, K., & Wonderlich, S. A. (2014). What is “grazing”? Reviewing its definition, frequency, clinical characteristics, and impact on bariatric surgery outcomes, and proposing a standardized definition. Surgery for Obesity and Related Diseases, 10(5), 973–982. https://doi.org/10.1016/j.soard.2014.05.002
Conceição, E. M., Mitchell, J. E., Machado, P. P. P., Vaz, A. R., Pinto-Bastos, A., Ramalho, S., Brandão, I., Simões, J. B., de Lourdes, M., & Freitas, A. C. (2017). Repetitive eating questionnaire [Rep(eat)-Q]: Enlightening the concept of grazing and psychometric properties in a Portuguese sample. Appetite, 117, 351–358. https://doi.org/10.1016/j.appet.2017.07.012
Conceição, E. M., Utzinger, L. M., & Pisetsky, E. M. (2015). Eating disorders and problematic eating behaviours before and after bariatric surgery: Characterization, assessment and association with treatment outcomes. European Eating Disorders Review, 23(6), 417–425. https://doi.org/10.1002/erv.2397
Courcoulas, A. P., Christian, N. J., Belle, S. H., Berk, P. D., Flum, D. R., Garcia, L., Horlick, M., Kalarchian, M. A., King, W. C., Mitchell, J. E., Patterson, E. J., Pender, J. R., Pomp, A., Pories, W. J., Thirlby, R. C., Yanovski, S. Z., & Wolfe, B. M. (2013). Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA - Journal of the American Medical Association, 310(22), 2416–2425. https://doi.org/10.1001/jama.2013.280928
Duarte, P. A. S., Palmeira, L. & Pinto-Gouveia, J. (2020) The Three-Factor Eating Questionnaire-R21: a confirmatory factor analysis in a Portuguese sample. Eating Weight Disorders 25, 247–256. https://doi.org/10.1007/s40519-018-0561-7
Galioto, R., Gunstad, J., Heinberg, L. J., & Spitznagel, M. B. (2013). Adherence and weight loss outcomes in bariatric surgery: does cognitive function play a role?. Obesity surgery, 23(10), 1703–1710. https://doi.org/10.1007/s11695-013-1060-6
Gill, H., Kang, S., Lee, Y., Rosenblat, J. D., Brietzke, E., Zuckerman, H., & McIntyre, R. S. (2019). The long-term effect of bariatric surgery on depression and anxiety. Journal of Affective Disorders, 246, 886–894. https://doi.org/10.1016/j.jad.2018.12.113
Gonçalves, M. R. dos S. (2020). Validação das propriedades psicométricas da urgência negativa (UPPS-P) para população portuguesa em diferentes grupos clínicos e comunitários.
Kalarchian, M. A., Marcus, M. D., Wilson, G. T., Labouvie, E. W., Brolin, R. E., & LaMarca, L. B. (2002). Binge eating among gastric bypass patients at long-term follow-up. Obesity surgery, 12(2), 270–275. https://doi.org/10.1381/096089202762552494
Keskitalo, K., Tuorila, H., Spector, T. D., Cherkas, L. F., Knaapila, A., Kaprio, J., Silventoinen, K., & Perola, M. (2008). The Three-Factor Eating Questionnaire, body mass index, and responses to sweet and salty fatty foods: a twin study of genetic and environmental associations. The American Journal of Clinical Nutrition, 88(2), 263–271. https://doi.org/10.1093/ajcn/88.2.263
Kochkodan, J., Telem, D. A., & Ghaferi, A. A. (2018). Physiologic and psychological gender differences in bariatric surgery. Surgical Endoscopy, 32(3), 1382–1388. https://doi.org/10.1007/s00464-017-5819-z
Leahey, T. M., Crowther, J. H., & Irwin, S. R. (2008). A cognitive-behavioral mindfulness group therapy intervention for the treatment of binge eating in bariatric surgery patients. Cognitive and Behavioral Practice, 15(4), 364–375. https://doi.org/10.1016/j.cbpra.2008.01.004
Lovibond S. H., Lovibond P. F. (1995) Manual for the depression anxiety stress scales. 2nd ed. Sydney: Psychology Foundation.
MacMahon, S., Baigent, C., Duffy, S., Rodgers, A., Tominaga, S., Chambless, L., De Backer, G., De Bacquer, D., Kornitzer, M., Whincup, P., Wannamethee, S. G., Morris, R., Wald, N., Morris, J., Law, M., Knuiman, M., Bartholomew, H., Davey Smith, G., Sweetnam, P., & Whitlock, G. (2009). Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. The Lancet, 373(9669), 1083–1096. https://doi.org/10.1016/S0140-6736(09)60318-4
McGuire, M. T., Jeffery, R. W., French, S. A., & Hannan, P. J. (2001). The relationship between restraint and weight and weight-related behaviors among individuals in a community weight gain prevention trial. International journal of obesity, 25(4), 574-580. https ://doi.org/10.1038/sj.ijo.08015 79
Mechanick, J. I., Youdim, A., Jones, D. B., Garvey, W. T., Hurley, D. L., McMahon, M. M., Heinberg, L. J., Kushner, R., Adams, T. D., Shikora, S., Dixon, J. B., & Brethauer, S. (2013). Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: Cosponsored by American association of clinical endocrinologists, the obesity society, and American society fo. Obesity, 21(SUPPL. 1), 1–27. https://doi.org/10.1002/oby.20461
Nasirzadeh, Y., Kantarovich, K., Wnuk, S., Okrainec, A., Cassin, S. E., Hawa, R., & Sockalingam, S. (2018). Binge eating, loss of control over eating, emotional eating, and night eating after bariatric surgery: results from the Toronto Bari-PSYCH Cohort Study. Obesity surgery, 28, 2032-2039. https://doi.org/10.1007/s11695-018-3137-8
Neumark-Sztainer, D., Wall, M., Guo, J., Story, M., Haines, J., & Eisenberg, M. (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later?. Journal of the American Dietetic Association, 106(4), 559-568. https ://doi.org/10.1016/j.jada.2006.01.003
Nicolau, J., Ayala, L., Rivera, R., Speranskaya, A., Sanchís, P., Julian, X., Fortuny, R., & Masmiquel, L. (2015). Postoperative grazing as a risk factor for negative outcomes after bariatric surgery. Eating Behaviors, 18, 147–150. https://doi.org/10.1016/j.eatbeh.2015.05.008
Odom, J., Zalesin, K. C., Washington, T. L., Miller, W. W., Hakmeh, B., Zaremba, D. L., Altattan, M., Balasubramaniam, M., Gibbs, D. S., Krause, K. R., Chengelis, D. L., Franklin, B. A., & McCullough, P. A. (2010). Behavioral predictors of weight regain after bariatric surgery. Obesity Surgery, 20(3), 349–356. https://doi.org/10.1007/s11695-009-9895-6
Pais-Ribeiro, J. L., Honrado, A. A. J. D., & Leal, I. P. (2004). Contribuição para o estudo da adaptação portuguesa das escalas de ansiedade, depressão e stress (EADS) de 21 itens de Lovibond e Lovibond. Psicologia, saúde & doenças, 2229-239.
Pinto-Bastos, A., de Lourdes, M., Brandão, I., Machado, P. P. P., & Conceição, E. M. (2019). Weight loss trajectories and psychobehavioral predictors of outcome of primary and reoperative bariatric surgery: a 2-year longitudinal study. Surgery for Obesity and Related Diseases, 15(7), 1104–1112. https://doi.org/10.1016/j.soard.2019.04.018
Rieber, N., Giel, K. E., Meile, T., Enck, P., Zipfel, S., & Teufel, M. (2013). Psychological dimensions after laparoscopic sleeve gastrectomy: reduced mental burden, improved eating behavior, and ongoing need for cognitive eating control. Surgery for Obesity and Related Diseases, 9(4), 569-573. https://doi.org/10.1016/j.soard.2012.05.008
Stunkard, A. J., & Messick, S. (1985). The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of psychosomatic research, 29(1), 71–83. https://doi.org/10.1016/0022-3999(85)90010-8
Vinogradov, S., Cox, P. D., & Yalom, I. D. (2003). Group therapy. In The American Psychiatric Publishing textbook of clinical psychiatry, 4th ed. (pp. 1333–1371). American Psychiatric Publishing, Inc.
Weineland, S., Arvidsson, D., Kakoulidis, T. P., & Dahl, J. (2012). Acceptance and commitment therapy for bariatric surgery patients, a pilot RCT. Obesity Research and Clinical Practice, 6(1), e21–e30. https://doi.org/10.1016/j.orcp.2011.04.004
Westenhoefer, J., Stunkard, A. J., & Pudel, V. (1999). Validation of the flexible and rigid control dimensions of dietary restraint. International Journal of Eating Disorders, 26(1), 53-64. https://doi.org/10.1002/(SICI)1098-108X(199907)26:1<53::AID-EAT7>3.0.CO;2-N
Whiteside, S. P., & Lynam, D. R. (2001). The Five Factor Model and impulsivity: using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30(4), 669-689. https://doi.org/10.1016/S0191-8869(00)00064-7