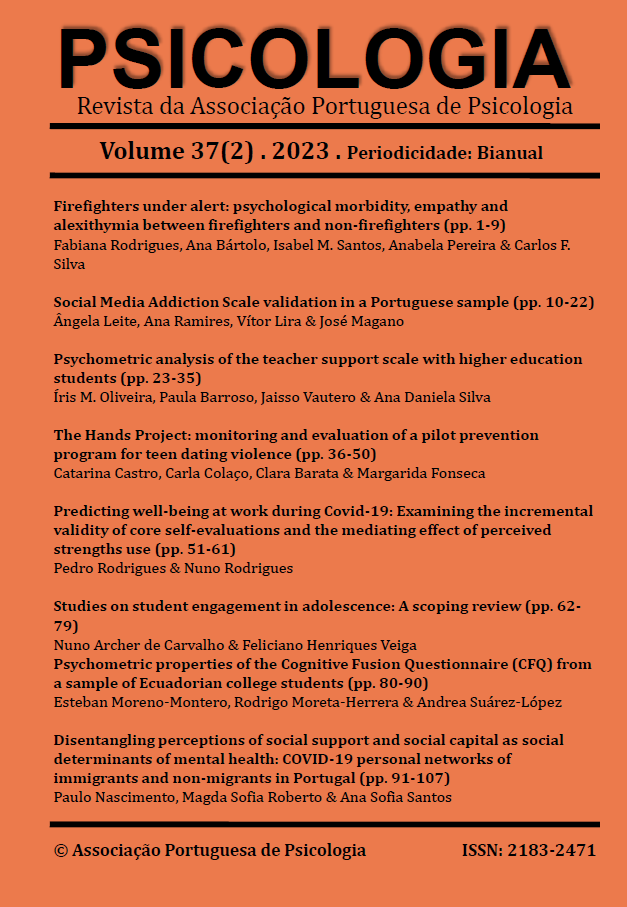
Disentangling perceptions of social support and social capital as social determinants of mental health: COVID-19 personal networks of immigrants and non-migrants in Portugal
DOI:
https://doi.org/10.17575/psicologia.1900Palavras-chave:
Mental Health, Social Support, Social Capital, Migrations, COVID-19Resumo
Social network changes may occur during disruptive events (e.g., COVID-19), especially with immigrants who need to rebuild networks, undermining their mental health. Study 1 (N =18) investigates immigrants' perceived changes before and during the pandemic in their networks, mental health, social support and social capital. Study 2 (N =53) examines the same in a sample of non-migrants. Convenience samples were collected online between July and November 2020, addressing participants' perceived health networks and mental health through name generators (alters’ names), name interpreters (attributes), position generator (social capital), and the Mental Health Inventory-5. E-net software assessed the network's efficiency and homophily. Study 1 results revealed immigrants reduced their mental health, and network changes by decreasing social support, efficiency and social capital. In study 2, non-migrant network changes were small, not compromising their efficiency and social capital. Contributions suggest the importance of health crisis management with actions to support migrant social networks.
Downloads
Referências
Arpino, B., & de Valk, H. (2018). Comparing life satisfaction of immigrants and natives across Europe: the role of social contacts. Social Indicators Research, 137, 1163–1184. https://doi.org/10.1007/s11205-017-1629-x
Borgatti, S. P. (2006). E-Network software for ego-network analysis [Computer software]. Analytic Technologies.
Brissette, I., Cohen, S., & Seeman, T. E. (2000). Measuring social integration and social networks. In S. Cohen, L. Underwood, & H. B. Gottlieb (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 53–85). Oxford University Press. https://doi.org/10.1093/med:psych/9780195126709.003.0003
Burt, R. S. (2000). The network structure of social capital. In R. Sutton & B. Staw (Eds.), Research in organizational behavior (pp. 345- 423). JAI Press.
França, T., & Oliveira, S. P. (2021). Brazilian migrant women as killjoys: Disclosing racism in “friendly” Portugal. Cadernos Pagu, 63, e216301. https://doi.org/10.1590/18094449202100630001
Gama, A., Rocha, J. V., Marques, M. J., Azeredo-Lopes, S., Pedro, A. R., & Dias, S. (2022). How did the Covid-19 pandemic affect migrant populations in Lisbon, Portugal? A study on perceived effects on health and economic condition. International Journal of Environmental Research and Public Health, 19(3), 1786. https://doi.org/10.3390/ijerph19031786
Gil, J. D. C., Aguiar, P. M. V., Azeredo-Lopes, S., Soares, P., Moura, H. S. D., Arcêncio, R. A., Goes, A. R. O., Gama, A., Pedro, A. R. S., Nunes, C., Moniz, A. M. F., Laires, P., Dias, S., F., Souza, R., M., P., Pinto, L. W., & Abrantes, A. (2022). Physical distancing and mental well-being in youth population of Portugal and Brazil during the COVID-19 pandemic. Portuguese Journal of Public Health, 40(2), 91-100. https://doi.org/10.1159/000525248
Godinho, M., Alarcão, V., Carreira, M., & Portugal, R. (2008, November 6-8). Existence of probable psychological distress in African and Brazilian immigrants in Portugal. [Poster presentation]. 16ª European Conference on Public Health, Lisbon, Portugal. http://uepid.wdfiles.com/local--files/projectos-de-investigacao/EUPHA_psychological%20distress.pdf
Jiang, H., & Carroll, J. (2009). Social capital, social network and identity bonds: a reconceptualization. Proceedings of the Fourth International Conference on Communities and Technology, USA, pp. 51-60. https://doi.org/10.1145/1556460.1556469
Johnson, C. M., Rostila, M., Svensson, A. C., & Engström, K. (2017). The role of social capital in explaining mental health inequalities between immigrants and Swedish-born: a population-based cross-sectional study. BMC Public Health, 17(1), 117. https://doi.org/10.1186/s12889-016-3955-3
Kawachi, I., & Berkman, L. F. (2001). Social ties and mental health. Journal of Urban Health volume, 78(3), 458–467. https://doi.org/10.1093/jurban/78.3.458
Kindler, M., & Wójcikowska-Baniak, K. (2019). (Missing) bridging ties and social capital? The creation and reproduction of migrants’ social network advantages: The case of Ukrainian migrants in Poland. Central and Eastern European Migration Review, 8(1), 95-116. https://doi.org/10.17467/ceemr.2019.02
Lecerof, S. S., Stafström, M., Westerling, R., & Östergren, P. O. (2016). Does social capital protect mental health among migrants in Sweden? Health Promotion International, 31(3), 644–652. https://doi.org/10.1093/heapro/dav048
Lee, S., Chung, J. E., & Park, N. (2016). Network environments and well-being: An examination of personal network structure, social capital, and perceived social support. Health Communication, 33(1), 22–31. https://doi.org/10.1080/10410236.2016.1242032
Lin, N., Cook, K., & Burt, R. S. (2001). Social capital: Theory and research. Aldine Transaction.
Liu, P. L., & Yeo, T. E. D. (2021). Weak ties matter: Social network dynamics of mobile media multiplexity and their impact on the social support and psychological well-being experienced by migrant workers. Mobile Media & Communication, 10(1), 76-96. https://doi.org/10.1177%2F20501579211001106
Lourel, M., Hartmann, A., Closon, C., Mouda, F., & Petric-Tatu, O. (2013). Social support and health: An overview of selected theoretical models for adaptation. In S. Chen (ed.), Social support, gender and culture, and health benefits (pp. 1–20). Nova Science Publishers.
Mair, C. A., & Thivierge-Rikard, R. V. (2010). The strength of strong ties for older rural adults: regional distinctions in the relationship between social interaction and subjective well-being. The International Journal of Aging and Human Development, 70(2), 119-143. https://doi.org/10.2190/ag.70.2.b
Majeed, M. T., & Ajaz, T. (2018). Social capital as a determinant of population health outcomes: A global perspective. Pakistan Journal of Commerce and Social Sciences, 12(1), 52-77. http://hdl.handle.net/10419/188335
Marsden, P. (2005). Recent developments in network measurement. In J. C. Scott & S. Wasserman (Eds.), Models and methods in social network analysis (pp. 8–30). Cambridge University Press.
McCarty, C., Lubbers, M. J., Vacca, R., & Molina, J. L. (2019). Conducting personal network research: A practical guide. The Guilford Press.
Meanley, S., Biernesser, C., O'Malley, T., Bear, T., & Trauth, J. (2020). Employing position generators to assess social capital and health: A scoping review of the literature and recommendations in future population health surveillance. Journal of Health Disparities Research and Practice, 13(3), 16–45.
Meng, X., & Xue, S. (2020). Social networks and mental health outcomes: Chinese rural–urban migrant experience. Journal of Population Economics, 33, 155–195. https://doi.org/10.1007/s00148-019-00748-3
Morina, N., Kip, A., Hoppen, T. H., Priebe, S., & Meyer, T. (2021). Potential impact of physical distancing on physical and mental health: a rapid narrative umbrella review of meta-analyses on the link between social connection and health. BMJ Open, 11(3), e042335. https://doi.org/10.1136/bmjopen-2020-042335
Passos, L., Prazeres, F., Teixeira, A., & Martins, C. (2020). Impact on mental health due to COVID-19 pandemic: Cross-Sectional study in Portugal and Brazil. International Journal of Environmental Research and Public Health, 17(18), 6794. https://doi.org/10.3390/ijerph17186794
Perry, B. L., & Pescosolido, B. A. (2010). Functional specificity in discussion networks: The influence of general and problem-specific networks on health outcomes. Social Networks, 32(4), 345–357. https://doi.org/10.1016/j.socnet.2010.06.005
Perry, B. L., & Pescosolido, B. A. (2012). Social network dynamics and biographical disruption: The case of “first-timers” with mental illness. American Journal of Sociology, 118(1), 134–175. https://doi.org/10.1086/666377
Perry, B. L., Pescosolido, B. A., Small, M. L., & McCranie, A. (2020). Introduction to the Special Issue on Ego Networks. Network Science, 8(2), 137–141. https://doi.org/10.1017/nws.2020.18
Platt, J., Keyes, K. M., & Koenen, K. C. (2014). Size of the social network versus quality of social support: which is more protective against PTSD? Social Psychiatry and Psychiatric Epidemiology, 49(8), 1279-86. https://doi.org/10.1007/s00127-013-0798-4
Posch, P., & Cabecinhas, R. (2020). Facing a pandemic away from home: Covid-19 and the Brazilian immigrants in Portugal. In I. Sirkeci & J. H. Cohen (Eds.), COVID-19 and Migration: Understanding the Pandemic and Human Mobility (pp. 105-117). Transnational Press London. http://hdl.handle.net/1822/69205
Putnam, R. D. (2000). Bowling alone: The collapse and revival of American community. Simon & Schuster.
Puyat, J. H. (2013). Is the influence of social support on mental health the same for immigrants and non-immigrants? Journal of Immigrant and Minority Health, 15(3), 598-605. https://doi.org/10.1007/s10903-012-9658-7
Ribeiro, J. L. P. (2001). Mental health inventory: Um estudo de adaptação. Psicologia: Saúde & Doenças, 2(2), 77-99.
Richardson, J., Postmes, T., & Stroebe, K. (2022). Social capital, identification and support: Scope for integration. PLoS ONE, 17(4), e0266499. https://doi.org/10.1371/journal.pone.0266499
Schulz, B., Horr, A., & Hoenig, K. (2017). The position generator in the NEPS (NEPS Survey Paper No. 23). Bamberg, Germany: Leibniz Institute for Educational Trajectories, National Educational Panel Study.
Sin, C., Antonowicz, D., & Wiers-Jenssen, J. (2021). Attracting international students to semi-peripheral countries: A comparative study of Norway, Poland and Portugal. Higher Education Policy, 34, 297–320. https://doi.org/10.1057/s41307-019-00135-3
Small, M. L. (2017). Someone to talk to. Oxford University Press.
Sweet, D., Byng, R., Webber, M., Enki, D. G., Porter, I., Larsen, J., Huxley, P., & Pinfold, V. (2018). Personal well-being networks, social capital and severe mental illness: Exploratory study. British Journal of Psychiatry, 212(5), 308-317. https://doi.org/10.1192/bjp.bp.117.203950
Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145-161. https://doi.org/10.1177%2F0022146510395592
Wellman, B. (2000). Partners in illness: Who helps when you are sick? In M. Kelner, B. Wellman, B.A. Pescosolido, & M. Saks (Eds.), Complementary and Alternative Medicine: Challenge and Change (pp. 143-162). Harwood Academic Publishers.